Gut Health and Pain – Part 2: The Gut-Brain Connection
Over the past decade there has been a lot of discussion about the importance of our gut. Our gut has been shown to be one of the keys to our overall health and wellbeing.
- It has been called our “second brain” due to the intricate nervous system (the enteric nervous system) it holds within in and how it communicates with our brain (the gut-brain axis).
- It has been shown to play a vital role in the production of serotonin, which has been one of the keys to understanding the role it plays in mood and sleep.
- It has been shown to play a vital role in our stress (hypothalamic pituitary adrenal (HPA) axis) and relaxation (through the vagus nerve) response.
- It is home to 100 trillion microorganisms and their genetic material, known as microbiome, and scientists are only just unlocking the potential of this live bacteria.
- Some of the most interesting areas being explored by scientists include the role our gut plays in immunity, inflammation and pain.
The following series “Gut Health and Pain” will take a look at the intricate world of our gut and unravel the mystery of why there is thousands journal articles being written each year about the health of our gut and the problems an unhealthy gut can cause. Welcome to Part 2 – The Gut-Brain Connection.
Part 2 – The Gut-Brain Connection
In our last article we discussed the importance of knowing your gut, the role our microbiome plays in our health and wellbeing, the link between gut microbiome and pain, the role our gut lining plays in our immune function, inflammation and pain. In this article we will discuss:
- What is the link between nutrition, mood and our pain?
- What is the gut-brain connection?
- What is the enteric nervous system?
- What is the link between mood and our gut?
- What is the link between nutrition, sleep and our pain?
- What is the gut-liver, gut-lung and gut-kidney axes?
What is the link between nutrition, mood and our pain?
Much like a car and the fuel it receives, your brain functions at its best when you give it a well-balanced diet. When it is deprived of good-quality nutrition it can affect your mental health and mood, sleep, physical health, immune system, and pain. When it comes to chronic pain and mental health, the statistics within Australia are alarming:
- Almost 50% of people living with chronic pain, also manage depression and anxiety
- Suicide is reported to be two to three times higher in those suffering chronic pain compared to the general population
- Major depression in patients with chronic pain is associated with reduced functioning, poorer treatment response and increased health care costs
- High rates of generalised anxiety disorder, post-traumatic stress disorder and substance misuse are also reported in people with chronic pain.
Scientists have been researching the role nutrition plays in mental health and chronic pain, and they believe the key lies in the gut-brain connection.
 What is the gut-brain connection?
What is the gut-brain connection?
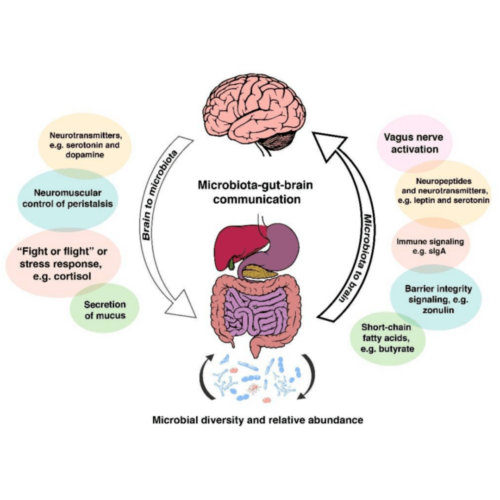
Our gut is intricately linked to our brain: the communication is bidirectional, meaning our brain communicates with our gut and vice versa. Our central nervous system (brain and spinal cord) communicate with the enteric nervous system (nervous system found in the gut) through a complex communication network known as the gut-brain axis, which involves the:
- Hypothalamic-pituitary-adrenal (HPA) axis – primarily involved in adaptive responses to stress including our limbic systems in our brain
- Immune cells (cytokine and chemokines)
- Vagus nerve – thought to be the main driver behind the mind-body connection
- Short chain fatty acids (brain food) – produced when the good gut bacteria ferment fibre in our colon
- Neurotransmitters (including serotonin our mood regulator) – chemical messenger which transmits signals from neuron to neuron, neuron to muscle or neuron to gland
- Gut permeability – transportation, absorption and balance of nutrients, immunity and tolerance of foreign substances
- Gut microbiome
- Autonomic nervous system (ANS) – driving both afferent (sensory) and efferent (motor) signals
What is the enteric nervous system?
The enteric nervous system (ENS) is a part of our autonomic nervous system (subconsciously controls and regulates our internal organs). Our gut has been labeled the “second brain” due to the intricate network of 50-100 million nerve cells which reside and communicate within it. The complex network of nerve cells allows us to monitor, communicate and integrate information from our gut to the rest of our bodies. It also controls: movement throughout the gut (peristalsis), exchange of fluids to assist with digestion (digestive juices) and maintains blood flow. The ENS is the heart of the gut-brain axis.
 What is the link between mood and our gut?
What is the link between mood and our gut?
There is an enormous volume of literature supporting how gut-health is linked to mood, with the key lying in the gut-brain axis. Researchers have identified how our gut produces almost 90% of our serotonin and how the millions of nerve cells that line the gut, don’t just help us digest our meal but also guide our emotions. Serotonin is a chemical released by our brain (neurotransmitter) that makes us feel happy, sleep better, modulates pain perception and helps us feel a general sense of wellbeing. Researchers have shown how an imbalance of serotonin and other neurotransmitters can significantly impact on mood, sleep and behaviours.
Some interesting areas of research in this area include:
- Researchers are also looking at how the gut-brain axis impacts on neurotransmitters, and vice versa. They believe the relationship between them may hold the key to decreasing symptomology and/or disease progression.
- Researchers are looking at the microbiome of animals, and how they produce a wide variety of neurotransmitters. There is accumulating evidence suggesting how neurotransmitters may be manipulated by introducing bacteria into the gut. This is an interesting area of research, with ongoing research into how neurotransmitter play a role in the perception of pain.
- Researchers are looking at the role our gut microbiome plays in mood. They believe that our gut microbiota influences brain function via the neuroimmune and neuroendocrine pathways, as well as the nervous system. That preliminary findings show marked changes to microbial diversity with people with mood disorders and believe that with more research, the brain-gut-microbiotia axis could be a promising target for disease diagnosis and therapeutic intervention.
What is the link between our nutrition, sleep and pain?
Much like the gut-brain axis, the link between sleep and pain is also biodirectional. Sleep disturbances are one of the most common causes of suffering among people living with chronic pain. Whilst pain itself directly affects getting and staying asleep, poor sleep feeds into the pain cycle, exacerbating pain. Research has shown poor sleep impacts on pain sensitivity, the duration of painful episodes and pain intensity. Poor sleep also has an impact on our mood, memory, energy levels and our ability to think rationally. Interestingly, researchers have also found another bidirectional relationship between nutrition and sleep:
- Sleep is directly related to our hormonal and metabolic processes (link): when we get good quality sleep it assists with:
- The balance within our body – hormones, metabolism, gut microbiome, neurotransmitters
- The reversal of the “stress response” on our body, primarily the HPA axis (which will discuss in the next article)
- The repair, recovery and rebooting of our brain and body
- Good quality sleep also has a direct impact on your “hunger hormones” (link):
- Increasing leptin, which is made by fat cells and assists with decreasing your appetite
- Decreasing ghrelin, which increases appetite and determines how quickly to turn hunger back on after a meal.
- Orexin neurons, which are responsible for the control of food intake and energy expenditure, motivation, and circadian rhythm of sleep and wake.
- Poor quality sleep is linked to diet-related behaviours and diseases (link):
- Irregular eating habits
- Snacking between meals
- Higher calorie meal choices
- An increased risk of type 2 diabetes and obesity
- Sleep impacts on our nervous system: Another interesting area of research is looking at how good quality sleep improves the waste removal system of the brain – the glymphatic system. Our brain accumulates waste products as a result of our metabolism; therefore, it is vital it is given the opportunity to remove this by a good quality night’s sleep.
- Gut bacteria influences sleep: Evidence suggests that the gut microbiome can influence the quality of sleep and our body clock’s natural rhythm. Experts believe that sleep is partially triggered by a drop in our body temperature. When we get our late night munchies, the snack we eat needs to be processed by our digestive system, which keeps our body temperature high and delaying the onset of sleep. Researchers have also found that much like us, our microbiome have an appetite which correlates with our 24hr clock (circadian rhythm). It is regulated by diet, time of meals, other microbiota and metabolic activity – all of which impacts on our immune and metabolic function.
The links between sleep, metabolism, microbiome, weight, nutrition and pain, are an area of medicine being widely researched. The question is, if a bad night sleep leads to increased pain and poor nutrition, could changing your diet improve your sleep and pain? If you want to learn more about good quality sleep, visit here

What is the gut-liver, gut-lung and gut-kidney axis’?
There are also three other axis’ that are being looked into by scientists, which only further explains the intricate connection the gut has with our body and brain, these are:
- Gut-liver axis: 70% of the blood flow to the liver, comes directly from the gut. Researchers are looking at how gut bacteria may role in the risk of developing fatty-liver disease.
- Gut-lung axis: Researches are currently looking at how gut microbiota impacts on asthma, chronic obstructive pulmonary disease, pneumonia and the development of some cancers.
- Gut-kidney axis: Researchers are looking at how diseased kidney affect the microbiota and how microbiota increase the toxins released in chronic kidney disease.
These intricate networks explain how the health of the gut can be linked to so many diseases within our body, and why we are only just at the tip of the iceberg in this fascinating field of medicine. This is also why an entire area of science known as psychobiotics has evolved, looking at the link between our live bacteria and gut, brain and health and how manipulating this may change our health and well-being.
To continue reading Part 3 – The Gut and Stress click here.
Additional references
- Journal Article: Eubiosis and dysbiosis: the two sides of the microbiota (article here)
- Article: Our gut microbiome is always changing; it’s also remarkably stable (link here)
- Book: Gut Health and Probiotics. The science behind the hype. Jenny Tschiesche
- Book: Rushing Woman’s Syndrome. The impact of a never ending to-do list on your health. Dr Libby Weaver
- Book: Gut. The inside story of our body’s most under-rated organ. Giulia Enders
- Book: The mind-gut connection. How the hidden conversation within our bodies impacts on our mood, our choices, and our overall health. Emeran Mayer, MD
- Journal Article: The Role of Gut Microbiota in Intestinal Inflammation with Respect to Diet and Extrinsic Stressors (article here)
- Journal Article: Gut microbiota functions: metabolism of nutrients and other food components (article here)
- Journal Article: Stress and the gut microbiota-brain axis (article here)
- Journal Article: Neurotransmitter modulation by the gut microbiota (article here)
- Journal Article: Current Understanding of Gut Microbiota in Mood Disorders: An Update of Human Studies (article here)
- AUSMED E-Learning: Gut Microbiota Health and Wellbeing (link here)
- Journal Article: A review of lifestyle factors that contribute to important pathways associated with major depression: Diet, sleep and exercise (article here)
- Journal Article: ‘Gut health’: a new objective in medicine? (article here)
- Journal Article: Impact of the gut microbiota on inflammation, obesity, and metabolic disease (article here)
- Journal Article: The association of sleep and pain: An update and a path forward (article here)
- Journal Article: The Important Role of Sleep in Metabolism (article here)
- Journal Article: Role of Sleep and Sleep Loss in Hormonal Release and Metabolism (article here)