Sleep Series – Part 1: Understanding Sleep
Sleep disturbances are one of the most common causes of suffering among people living with chronic pain. Whilst pain itself directly affects getting and staying asleep; poor sleep feeds into the pain cycle, only exacerbating pain.
In this Sleep Series we will look at: understanding sleep, understanding sleep disturbances and how you can get a better night’s sleep. Welcome to Part 1: Understanding Sleep.

Part 1: Understanding Sleep
All living creatures with brains sleep; in the animal kingdom sleep is preserved for the time after all biological needs are met (food, water, safety). Sleep is a period when our bodies and brains appear to rest, recover, repair and reboot.
There is currently an endemic of sleep issues around the world and it is seen as one of the world’s most curable disease; with people living with chronic pain being disproportionately affected by these issues, with almost 50% dealing with insomnia. Understanding what sleep is and why we need it, can help us to understand the toll a bad night sleep takes on us and how to get a better night’s sleep.
In this article we will discuss:
- What is sleep?
- What is our sleep-wake cycle?
- What is our circadian rhythm?
- How does our brain help us sleep?
- What are the phases of sleep?
- Which is more important, quality or quantity?
- Why is sleep important?
- What is the link between sleep and pain?
- What is the link between sleep and diet?
What is sleep?
Sleep is a period of time when our eyes are closed, bodies and muscles are relaxed, and our brain appears to shut off. Surprisingly, this is far from the whole story or truth. Our brains and the cells within our bodies are actually quite active whilst we sleep, completing many vital functions, including:
- Consolidating memories and storing it away into our long-term memory (learn more here)
- Restoring our ability to concentrate and pay attention (learn more here)
- Repairing muscles and allowing them to recover (learn more here)
- Regulating our metabolism, hunger and cravings (learn more here)
- Processing our emotions (learn more here)
- Restoring our well-being (learn more here)
In order to fall asleep we have two systems in our body that operate 24hours a day:
- Our sleep-wake cycle – how long we have been awake and when it is time to sleep. It accounts for our sleep drive.
- Our circadian rhythm – our sleepiness and wakefulness over a 24hour period. It rises and falls over the 24hour period, with the strongest drive at 2-4am and a weaker drive again at 1-3pm.
 What is our sleep-wake cycle?
What is our sleep-wake cycle?
Our sleep-wake cycle is how our body monitors the length of time we have been awake and when it is time to go to sleep.
Our sleep-wake cycle is organised by:
- Darkness: which marks the release of melatonin and the cascade of bodily processes that induce sleepiness (learn more here)
- Hormones changes at night: such as serotonin which drops, melatonin which increases and adenosine which gradually increases every hour we are awake, initiating the onset of sleep (learn more here)
- Hormones changes in the morning: which change approximately 90mins before we wake, such as melatonin which drops and cortisol and serotonin which increases (learn more here)
- Body temperature: which decreases as we sleep and increases as we wake (learn more here)
- Sunlight: which is registered through our eyes (even when closed) and signals that it is time to wake up, this also triggers the release of serotonin (learn more here)
Interestingly, the serotonin dip we experience of a night is why we find ourselves looking for high carbohydrate snacks. Carbohydrates can assist in the production of serotonin and give us a burst of energy when we are tired. This dip in serotonin can also explain why our moods take a dip and we can find ourselves getting more irritable later in the evening. The dip in serotonin plays a crucial role in sleep; so take cravings and irritability as a sign it’s time to go to bed.
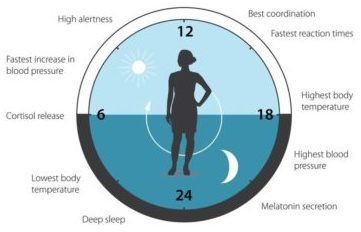 What is our circadian rhythm?
What is our circadian rhythm?
Our circadian rhythm monitors our sleepiness versus wakefulness over a 24hour period. It rises and falls throughout this 24hr period, and explains why we feel often tired around 1-3pm.
Our individual circadian rhythm is something quite unique to us:
- It dictates if we are an early-bird “lark” or night-owl
- It dictates the peaks and troughs of alertness and sleepiness
- It dictates how much sleep we need to feel refreshed and alert throughout the day (quality and quantity)
Interesting, there has been some research into circadian rhythms and they have noted that early-birds may have a 24hour clock that runs slightly faster and night-owls, one which runs slightly slower. This accounts for the differences in bedtime and waking times, it also accounts for why it is so difficult to wake up earlier than you usually do when you are a night owl. A good tip for when you need to wake earlier is to sit in the sunlight, this switches off melatonin (our sleepy hormone) and increases the release of serotonin.
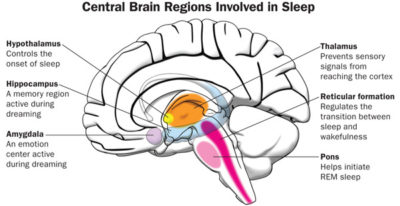 How does our brain help us sleep?
How does our brain help us sleep?
Our brain organises our sleep-wake cycle using external cues such as sunlight which regulate hormones such as serotonin (our happy hormone) and melatonin (our sleep hormone). The parts of our brain involved in sleep include:
- The thalamus: which shuts off incoming signals while we sleep
- The cerebellum: active during dreaming
- The amygdala: what makes us cranky when we haven’t slept enough
- The hypothalamus: controls our body’s cardiac rhythm
- The hippocampus: transfers short too memories to long term
- The prefrontal cortex: active during lucid dreaming.
Learn more about the research looking at the relationship between the brain and sleep here.
Video courtesy of NBC News
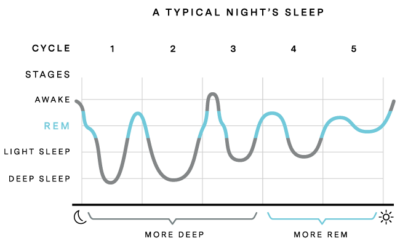 What are the phases of sleep?
What are the phases of sleep?
Many people believe good quality sleep is one solid sleep, but this is actually not the case. Normal sleep involves periods of light sleep, deeper sleep (also known as slow wave sleep), dreaming (rapid eye movement) and waking. It is normal to move through each of these stages, including waking, many times through-out the night.
Our sleep is divided into REM and non-REM sleep:
- Rapid Eye Movement (REM) Sleep: REM sleep is where our “story-like” dreams occur and is involved in emotional memories being processed and ensuring our psychological health. The reason we don’t act out the realness of our dreams is because we are effectively “paralysed” during this stage, apart from our eyes twitching and jerking back and forth. Note, there are some sleep disorders which suppress this “paralysis” (learn more here)
- Non-REM Sleep: Non-REM sleep is split into several stages:
- Stage 1 (Light Sleep): our transition between wake and asleep, where you are easily woken, muscles contract and often this is the stage where you dip in and out of sleep and feel like you have been awake for hours
- Stage 2-3 (Light Sleep): we spend a majority of our night in this stage and it is believed to be where our memories are consolidated
- Stage 4 (Heavy/Slow-Wave Sleep): the first third of our night is spend predominately in this stage and is closely linked to restorative processes and feelings of well-being.
Approximately every 90-120mins we cycle through these sleep stages and being awake, with more time being spend in deep sleep at the beginning of the night and more time being spent in REM in the morning. This is why when we “sleep-in” in the morning we often have vivid dreams.
Which is more important, quality or quantity?
In order for your body to get the benefits of sleep, you need to get the “right amount” per night. This amount changes depending on your age and how much growth your body is going through.
The “right amount” is a combination of the time you spend asleep versus the amount on time you are awake in bed (sleep efficiency) and how you wake in the morning. The time you spend asleep allows for the right proportion and distribution of each of your sleep stages – this quality and quantity are something quite unique to you.
Sleep efficiency is how long you spend asleep compared with how long you spend awake in bed during the night either trying to fall asleep. Good sleep efficiency is roughly 85% (to calculate your sleep efficiency visit here).
How you wake in the morning, is how know if you have had the right amount and good sleep efficiency; if you are not refreshed, awake, alert and ready for the day ahead, then the chances are it wasn’t the right quantity or quality.
The Australian Government recommends an average of 7-9hrs, but this amount changes throughout our lifespan:
- At 0-3 months, we need 14-17hrs
- At 4-11 months, 12-15hrs
- At 3-5 years, 10-13hrs
- At 6-13 years, 9-11hrs
- At 14-18 years, 8-10hrs
- From 25yrs, 7-9hrs
The recommended time frames for sleep do not take into account the number of people with medical conditions which struggle with sleep, as a result of their condition. This is why, focusing on how you wake in the morning and your sleep efficacy can be a better guide to knowing whether you have had sufficient sleep over night.
Why is sleep important?
Have you ever wondered why your pain is worse, or why you are irritable and hungry? The answer may be in your sleep.
Other than all the brain and cellular functions which occur whilst we sleep; sleep also plays a vital role in our:
- Memory (learn more here)
- Conversation skills (learn more here)
- Stress levels (learn more here)
- Self-control (learn more here)
- Ability to maintain healthy habits (learn more here)
- Thought processing (learn more here)
- Risk taking behaviour (learn more here)
- Ability to focus (learn more here)
- Emotion regulation (learn more here)
- Ability to be compassionate, empathetic and show care towards others (learn more here)
- Hunger and appetite (learn more here)
- Hormones and metabolism (learn more here)
- Pain sensitivity and tolerance (learn more here)
- Immune system and the production of cytokines (learn more here)
- Glymphatic system and removal of waste products form the brain and nervous system (learn more here)
- Gut health and the microbiome (learn more here)
 What is the link between sleep and pain?
What is the link between sleep and pain?
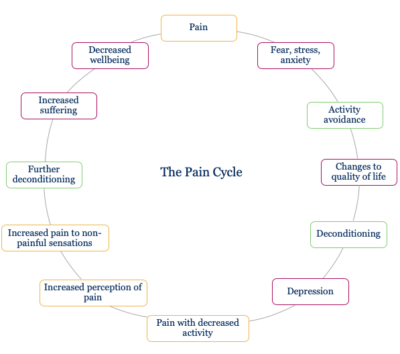
The pain cycle is a concept which explains the flow-on effects of pain on every aspect of a person’s life. It looks at how pain changes:
- our ability to exercise
- our mood
- our sleep
- our diet
It shows how the longer pain continues the greater the cascade of issues, including issues with work, finances and relationships. Often looking at the enormity of this cycle is too much to take on. Active self-management strategies in pain management look at each issue independently; working on simple strategies to tackle each issue one-by-one.
Insufficient long-term sleep has a similar cycle to the pain cycle. A poor night sleep significantly impacts on mood, concentration, motivation and willpower. It also impacts on pain. Research has shown that lack of sleep influences tolerance and sensitivity to pain; which, in short means our pain is more painful and causes us more distress, when we do not get the right amount of sleep.
Much like chronic pain management, sleep disturbances often require a multidisciplinary approach to manage them. Often, the input of a GP, Pain Specialist, Clinical Psychologist and/or Psychiatrist, Physiotherapist, Sleep Specialist and Dietitian can assist you with getting a better quality sleep.
In our next article we will look at one of the most common sleep problems – Insomnia – and some other causes of a bad night sleep.
What is the link between sleep and diet?
Sleep disturbances are one of the most common causes of suffering among people living with chronic pain. Whilst pain itself directly affects getting and staying asleep, poor sleep feeds into the pain cycle, exacerbating pain. Research has shown poor sleep impacts on pain sensitivity, the duration of painful episodes and pain intensity.
Interestingly, researchers have also found another bidirectional link between nutrition and sleep:
- Sleep is directly related to our hormonal and metabolic processes (link): when we get good quality sleep it assists with:
- The balance within our body – hormones, metabolism, gut microbiome, neurotransmitters
- The reversal of the “stress response” on our body, primarily the HPA axis (learn more about the HPA axis here)
- The repair, recovery and rebooting of our brain and body
- Good quality sleep also has a direct impact on your “hunger hormones” (link):
- Increasing leptin, which is made by fat cells and assists with decreasing your appetite
- Decreasing ghrelin, which increases appetite and determines how quickly to turn hunger back on after a meal.
- Orexin neurons, which are responsible for the control of food intake and energy expenditure, motivation, and circadian rhythm of sleep and wake.
- Poor quality sleep links to our weight and diet (link):
- Irregular eating habits
- Snacking between meals
- Higher calorie meal choices
- An increased risk of type 2 diabetes and obesity
- Sleep impacts on our nervous system: Another interesting area of research is looking at how good quality sleep improves the waste removal system of the brain – the glymphatic system. Our brain accumulates waste products as a result of our metabolism; “slow wave sleep”, our deepest sleep is how we remove these waste products from our brain.
The links between sleep, metabolism, microbiome, weight, nutrition and pain, are an area of medicine being widely researched. To continue reading our Sleep Series – Part 2: Understanding Sleep Problems, click here
Additional References
- Book: How to Sleep Well. The science of sleeping smarter, living better and being more productive. Dr Neil Stanley
- Book: Fast Asleep. How to get a really good night’s rest. Dr Michael Mosley
- Book: Sleep Well Every Night. A new approach to getting a good night’s sleep. Glenn Harrold
- Book: The Sleep Coach. Dr Sarah Jane Arnold
- Book: This Book Will Make You Sleep. Dr Jessamy Hibberd and Jo Usmar
- Journal Article: Measuring Sleep Efficiency: What Should the Denominator Be? (link here)
- Journal Article: From Lark to Owl: developmental changes in morningness-eveningness from new-borns to early adulthood (link here)
- Journal Article: Circadian system, sleep and endocrinology (link here)
- Journal Article: Cross‐talk between circadian clocks, sleep‐wake cycles, and metabolic networks: Dispelling the darkness (link here)
- Journal Article: Performance and Mood Following Variations in the Length and Timing of Sleep (link here)
- Journal Article: About Sleep’s Role in Memory (link here)
- Journal Article: Interactions between sleep, stress, and metabolism: From physiological to pathological conditions (link here)
- Journal Article: Interactions between sleep habits and self-control (link here)
- Journal Article: Sleep, Self-Regulation, Self-Control and Health (link here)
- Journal Article: Too exhausted to go to bed: Implicit theories about willpower and stress predict bedtime procrastination (link here)
- Journal Article: Changes in cognitive processing following short-term cumulative partial sleep deprivation and recovery oversleeping (link here)
- Journal Article: Sleep duration and risk-taking in adolescents: A systematic review and meta-analysis (link here)
- Journal Article: Sleep and emotions: A focus on insomnia (link here)
- Journal Article: The effects of sleep deprivation on emotional empathy (link here)
- Journal Article: Nocturnal levels of ghrelin and leptin and sleep in chronic insomnia (link here)
- Journal Article: Short Sleep Duration Is Associated with Reduced Leptin, Elevated Ghrelin, and Increased Body Mass Index (link here)
- Journal Article: Metabolic consequences of sleep and sleep loss (link here)
- Journal Article: The Association of Sleep and Pain: An Update and a Path Forward (link here)
- Journal Article: Sleep and pain (link here)
- Journal Article: Sleep and Pain: Interaction of Two Vital Functions (link here)
- Journal Article: The Effects of Sleep Deprivation on Pain (link here)
- Journal Article: Duration of sleep contributes to next-day pain report in the general population (link here)
- Journal Article: Sleep and pain sensitivity in adults (link here)
- Journal Article: Sleep difficulties, pain and other correlates (link here)
- Journal Article: Do Sleep Disorders Contribute to Pain Sensitivity? (link here)
- Journal Article: The role of sleep in pain and fibromyalgia (link here)
- Journal Article: Negative Mood Mediates the Effect of Poor Sleep on Pain Among Chronic Pain Patients (link here)
- Journal Article: Intraindividual Variability in Daily Sleep and Pain Ratings Among Chronic Pain Patients: Bidirectional Association and the Role of Negative Mood (link here)
- Journal Article: Does Effective Management of Sleep Disorders Improve Pain Symptoms? (link here)
- Journal Article: Total sleep deprivation increases pain sensitivity, impairs conditioned pain modulation and facilitates temporal summation of pain in healthy participants (link here)
- Journal Article: Nutrition, sleep and recovery (link here)
- Journal Article: Sleep and recovery (link here)
- Article: Sleep Deficit: The Performance Killer (link here)
- Website: Quizlet (link here)
- Website: Oura (link here)
- Website: Nobel Prize for Medicine goes to scientists studying circadian rhythms (link here)