The 12 Pillars of Wellbeing for Managing Pain
The World Health Organisation (WHO) defines health as ‘a state of complete physical, mental and social wellbeing and not merely the absence of disease or infirmity’ (WHO, 1948). “This is consistent with the biopsychosocial model of health, which considers physiological, psychological and social factors in health and illness, and interactions between these factors. The WHO definition links health explicitly with wellbeing, and conceptualises health as a human right requiring physical and social resources to achieve and maintain.” I Crinson 2007, Lina Martino 2017.
“Positive psychology is the scientific study of what makes life most worth living” (Peterson, 2008). According to positive psychology, wellbeing includes the five elements of PERMA:
- Positive emotions: feeling good.
- Engagement: being completely absorbed in your passions and the activities you do.
- Relationships: being meaningfully connected to others.
- Meaning: having a purposeful existence.
- Achievement: feeling a sense of accomplishment and success.
Wellbeing explores the deep peace, happiness and satisfaction we find in finding purpose, accomplishing meaningful activities and connecting with others. Its helps us build support systems, believe in ourselves and our ability to cope, and to stay resilient through challenges. A strong sense of wellbeing helps protect us from isolation, loneliness, hopelessness, depression and anxiety.

Wellbeing – Mental, Physical & Emotional Health.
What are the 12 pillars of wellbeing for managing pain?
The 12 pillars of wellbeing for managing chronic pain were developed as complimentary strategies for actively self-managing chronic pain. This program was launched in January 2020 on our Facebook and Instagram pages and introduces practical steps to managing chronic pain, health and wellbeing. Each topic is linked to media releases, published articles, clinical research, books, podcasts, video’s and new concepts in pain management. This article summaries why each of the 12 pillars of wellbeing is important for managing chronic pain.
According to an article published by Adriaan Louw for the Institute for Chronic Pain, people living with pain are interested in learning about their condition; what is going on, why it is occurring and how to manage it. This is the basis on therapeutic neuroscience education (TNE) and active self-management. A large volume of high-quality studies have shown that teaching people about the neuroscience of pain shows immediate and long-term changes including pain levels decreasing, function improving, patient’s spend less money on medical tests and treatments and wellbeing improves. Learning more about chronic pain ensures a reduction in the suffering associated with living with chronic pain and improvement in quality of life. To learn more about understanding pain click here.
The human body is designed to move and be active. When chronic pain causes a reduction in movement, a host of other health problems may arise making the recovery process more difficult and lengthy. When people experience chronic pain, there is a natural tendency to be over-protective and avoid movement. When muscles are inactive, they quickly deteriorate and joints become stiff, which can cause increased pain and reduced bodily function. Keeping physically active through healthy movement will ensure that chronic pain isn’t exacerbated by immobility. To learn more about healthy movement click here and to learn more about the basics of exercise click here.
 Sleep
Sleep
Getting good quality sleep is important for the body’s restorative functions. A large majority of patients who experience chronic pain naturally find it difficult to fall asleep and stay asleep. Sleep disturbances resulting from chronic pain may make coping with pain more difficult. Although frustrating, it is important to be reassured that lack of sleep can be managed and the main focus should be on the quality of sleep, rather than the quantity. Establishing a good sleep routine will assist in minimising sleep disturbances. To learn more about good quality sleep click here.
Rest
In a world that now operates 24hrs a day, many of us no longer take the time to rest. Being constantly on the go, with an infinite to-do list, can lead to a constant state of stress in our minds and bodies. This constant state of stress can significantly impact on wellbeing and pain. Rest allows our mind and body to stop, be free of demands and pressures. Rest is a time where we are able to relax, restore and unwind. Rest is the absence of activity. Ensuring the right balance between movement and rest is crucial for actively self-managing pain and building up activity tolerances. To learn more about pacing and rest click here.
Relaxation
Relaxation differs from rest because it often involves concentration. Relaxation activates the parasympathetic nervous system – our “rest and digest” system – which has the opposite effects to our stress response. Current evidence suggests relaxation techniques such as mindful meditation, deep breathing and guided meditations, can assist with managing symptoms associated with chronic pain. To learn more about relaxation techniques click here.

Nutrition is more than just managing your weight. What we eat becomes the foundation to our overall health and wellbeing, because it makes up the structure, function and integrity of every single cell in our body. Good quality nutrition has an impact on our mood, sleep and pain. When nutrition is poor it can have an impact on our immune system, making us more prone to illness and potentially contributing to pain; on inflammation within our body, which can contribute to pain and recovery; and our general feelings of wellbeing (mental, emotional and physical). To learn more about nutrition and pain click here.

Your gut plays host to 40 trillion microbiome (fungi, bacteria and other organisms) which help with digestion, your immune system, assisting with essential nutrient production your body can’t produce on it’s own, as well as determining which parts of your DNA to keep dormant or replicate. These microbes play an important role in appetite, allergies, metabolism, mood, neurological function, mental health and some types of pain. Emerging research in this field suggests a well balanced diet contributes to good gut health and potentially to pain management. To learn more about gut health and pain click here.

3.24 million Australian’s are currently living with chronic pain; with research suggesting that social isolation is responsible for decreased quality of life; greater reliance on GP services (primarily for the purpose of social issues); greater pain interference; and decreased physical function. Almost 40% of people living with chronic pain also experience depression and anxiety. The social consequence of chronic pain has been widely studied, with the most prominent determining factor of suffering and distress relating to the disruption of social relationships, not the physical impairment caused by pain.
Social wellbeing– or connection with others – is a large contributor to understanding and managing pain effectively. Research suggests that support, community engagement and social connection leads to positive wellbeing; heightened self-esteem and self-confidence; improved sense of control and self-efficacy; greater resilience and determination; improved mental and emotional health, including decreased levels of depression and anxiety; greater coping abilities; and may also improve the effectiveness of pain-related treatments. To learn more visit here

Social prescribing is a relatively new and innovative way of addressing the broader social aspects of wellbeing and health, associated with chronic diseases. It has come as a result of the ever-increasing social issues of loneliness, isolation and associated mental health issues that are related to living with chronic illness. Social prescribing has the primary aim of building local social connections through engaging with groups such as sports, arts, cooking, religious, walking, gardening and voluntary. These social engagements lead to heightened self-esteem and self-confidence; improved sense of control and empowerment; improved physical, emotional and mental wellbeing; and decreased levels of anxiety and depression.
Volunteering in particular can offer a large array of benefits including, making new friends; learning new skills; increasing your ability to re-join the workforce; a sense of gratitude and fulfilment for giving to those in need; enhances mental and physical health; a sense of purpose; it improves your social and relationship skills; it links you with like-minded people; it reduces depression, stress and anxiety levels; it improves your confidence levels; it is great for improving mobility and function; it allows you to test out new career opportunities; and it reduces loneliness and isolation. To learn more visit here

People who have found their strengths and passion, and use them for a purpose greater than themselves are some of the happiest people amongst us, according to positive psychologists. When we find our strengths and passion we experience more positive emotions, find purpose and meaning, feel a sense of engagement, foster healthier relationships and enhance our quality of life. Engaging in activities that utilise our strengths and passions, enhance feelings of self-belief (self-efficacy), resilience and self-confidence; allowing us to feel a sense of purpose and meaning in our life.
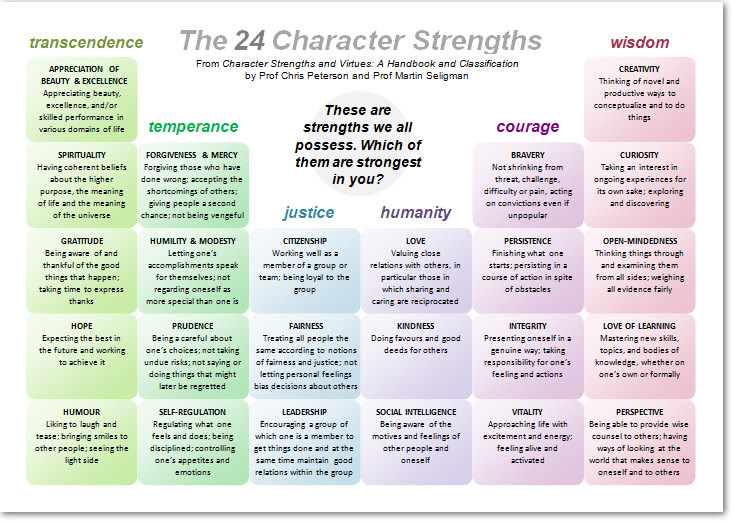
Image courtesy of This Way Up
According to Psychologist Martin Seligman, when we use our strengths and find our passion we feel like the real us, learning quickly, feeling energised, and a sense of joy and enthusiasm. We can also experience a mindfulness moment known as “flow”. Flow was first scientifically defined by Mihaly Csikszentmihalyi, he observed it as a period of time where you lost all sense of time and attention to yourself, you were intensely focused on the present moment and felt a sense of personal control over the situation. This experience allows a sense of calm, mindfulness and immense satisfaction and peace; and has been linked to many positive emotions, including joy, self-belief, self-compassion, self-confidence and enthusiasm. To learn more visit here.

According to Kabat-Zinn (2003), mindfulness is defined as the “awareness that emerges through paying attention on purpose, in the present moment, and non-judgmentally to the unfolding of experience moment to moment.” Mindfulness-based cognitive training can be effective in regulating attention to pain by distracting and distancing from the physical feeling of pain (Garland et al., 2009). There is emerging research looking at how practising mindfulness can change brain function and pain. To learn more about mindfulness and the brain click here.
According to the experts, gratitude is defines as “… an affirming of goodness or “good things” in one’s life and the recognition that the sources of this goodness lie at least partially outside the self” (Dr Robert Emmons and Dr Robin Stern); “The appreciation of what is valuable and meaningful to oneself; it is a general state of thankfulness and/or appreciation” (Dr Randy and Dr Lori Sansone); and “Involving a life orientation towards noticing and appreciating the positive in life” (Dr. Alex Wood).
Research has shown that practicing gratitude can change the plasticity of the brain, improve physical and emotional health, enhance empathy, improve sleep, enhance self-esteem and increase resilience. Regular focusing on the positive, what you can do and what you have, can have a significant impact on wellbeing, function, mood and pain. Learn more about gratitude and happiness research here.

According to the Merriam-Webster Dictionary, empathy is “the action of understanding, being aware of, being sensitive to, and vicariously experiencing the feelings, thoughts, and experience of another of either the past or present without having the feelings, thoughts, and experience fully communicated in an objectively explicit manner; also : the capacity for this”.
There has been many studies that look at the impact of receiving empathy when living with pain and the effects this has on the levels of pain experienced. Body and Mind conducted 2 experimental studies with romantic couples and the impact romantic partners might have on pain. Both experiments highlighted how receiving empathy from a romantic partner helped lessen the pain felt. This may be due to emotion regulation, which is experienced as a result of intimacy, closeness and acceptance, which may reduce the threat value in a pain-provoking situation. Ensuring family, friends and partners understand chronic pain allows a greater level of empathy towards those living with chronic pain, which may lead to a reduction in the pain experienced.
Empathy can also be helpful in Mindfulness-Based Stress Reduction (MBSR) techniques. Which have shown how patients can change their perception of pain through developing a capacity to observe their thoughts and feelings from a detached perspective. This perspective shift requires empathy, allowing them to depersonalise and detach from the experience, almost as if it were occurring to another person. Learn more about MBSR techniques here.

Support can come in a variety of forms when you are living with chronic pain, it may be the kindness of a stranger, to the assistance of someone else living with pain, to the financial and health assistance given by the government and healthcare team treating you. Whatever the means of support, it allows you to connect with others and reduce the detrimental impact of isolation and loneliness.
Support groups offer friendships; information; tools and strategies for managing pain; an opportunity to share experiences and stories; an ability to learn new skills and techniques; and a safe and empathetic environment surrounded by people who truly understand what living with chronic pain is like. Support groups can be found in every city and town around Australia and can be in-person; online or via phone. For example the Pain Link Helpline is a call back service that offers lifeline to people living with chronic pain, particularly in rural and regional areas of Australia. Phone Number: 1300 340 357. To learn more visit here
